Neurologijos seminarai ISSN ISSN 1392-3064 / eISSN 2424-5917
2023, 27(98), pp. 246–251 DOI: https://doi.org/10.15388/NS.2023.27.98.5
Originalus mokslinis straipsnis / Original Research
A. Atkočiūnas
Outpatient Consultation Department, Mykolas Marcinkevičius Hospital, Vilnius, Lithuania.
A. Šimkutė
Faculty of Medicine, Vilnius University, Vilnius, Lithuania.
R. Mameniškienė
Clinic of Neurology and Neurosurgery, faculty of Medicine, Vilnius University, Vilnius, Lithuania.
Summary. Background and aim: Carpal tunnel syndrome (CTS) is a compressive neuropathy caused by compression of the median nerve in the carpal tunnel. It is the most common entrapment neuropathy. According to different studies, the prevalence of CTS among adults (15–65 years old) in Western Europe ranged from 0.29% to 43%. CTS affects middle-aged active workers and is associated with high healthcare costs and a hefty economic burden. It is thus essential to diagnose CTS early and refer the patient to further investigation and treatment. In this study, we aimed to evaluate the accuracy of the clinical CTS diagnosis before the nerve conduction studies were performed on the referred patients.
Methods: The concordance of clinical diagnoses was assessed by comparing referral diagnoses with diagnoses confirmed by electroneuromyography. All the patients referred for electroneuromyography to Mykolas Marcinkevičius Hospital between August 2023 and February 2024 were included in this research. The age, sex, referral and final diagnoses of the enrolled patients were taken from their outpatient charts. The obtained data were summarized and processed with Microsoft Office Excel 365, and the data analysis was performed with IBM SPSS Statistics.
Results: The most common reasons that patients were referred to perform NCS were suspected carpal tunnel syndrome (30.7%), cubital tunnel syndrome (13.5%), other upper extremity mononeuropathies (16.2%), and polyneuropathies (15.5%). The most common diagnosis after consultation was carpal tunnel syndrome (42.6%), followed by pathologies of nerve roots or plexuses (14.5%). Out of 91 patients referred to electroneurography due to suspicion of CTS, 67 (73.6%) were confirmed cases, whereas, for 12 (13.2%) patients, no abnormalities were detected during NCS.
Conclusion: Our analysis supports the theory that the electrodiagnostic examination is essential to specify and confirm the diagnosis of CTS, thus avoiding hyperdiagnosis and preventing patients from excessive surgical treatment.
Keywords: Nerve conduction studies, Electroneuromyography, Carpal tunnel syndrome
Santrauka. Įvadas ir tikslas. Riešo kanalo sindromas (RKS) yra kompresinė neuropatija, kurią sukelia vidurinio nervo suspaudimas riešo kanale. RKS yra labiausiai paplitęs iš kompresinių neuropatijų. Įvairių tyrimų duomenimis, RKS paplitimas tarp suaugusiųjų (15–65 metų) Vakarų Europoje svyravo nuo 0,29 % iki 43 %. Kadangi RKS paveikia vidutinio amžiaus aktyvius darbuotojus, jis yra susijęs su didelėmis sveikatos priežiūros išlaidomis ir ekonomine našta. Svarbu anksti diagnozuoti RKS ir siųsti pacientą tolesniam ištyrimui ir gydymui. Šiuo tyrimu siekėme įvertinti klinikinės RKS diagnozės tikslumą prieš atliekant nervų laidumo tyrimus pacientams.
Metodai. Buvo vertinamas klinikinių diagnozių atitikimas lyginant siuntimo diagnozes su diagnozėmis, patvirtintomis elektroneuromiografijos tyrimu. Į tyrimą įtraukti visi pacientai, siųsti elektroneuromiografijos tyrimui nuo 2023 m. rugpjūčio mėn. iki 2024 m. vasario mėn. Pacientų amžius, lytis, siuntimo ir galutinė diagnozės buvo paimti iš pacientų ambulatorinių kortelių. Gauti duomenys buvo apibendrinti ir apdoroti „Microsoft Office Excel 365“, o duomenų analizė atlikta „IBM SPSS Statistics“.
Rezultatai. Dažniausios priežastys, dėl kurių pacientai buvo siųsti atlikti elektroneurografiją, buvo įtariamas riešo kanalo sindromas (30,7 %), alkūninio kanalo sindromas (13,5 %), kitos viršutinių galūnių mononeuropatijos (16,2 %) ir polineuropatijos (15, 5 %). Dažniausia diagnozė po konsultacijos buvo riešo kanalo sindromas (42,6 %), paskui – nervų šaknelių ar rezginių patologijos (14,5 %). Iš 91 paciento, atsiųsto elektroneurografijai dėl įtariamo RKS, 67 (73,6 %) pacientams RKS buvo patvirtintas, o 12 (13,2 %) pacientų elektroneurografijos metu kliniškai reikšmingų pakitimų nenustatyta.
Išvada. Mūsų tyrimas rodo, kad elektroneurografijos tyrimas yra būtinas norint patikslinti ir patvirtinti RKS diagnozę, siekiant išvengti hiperdiagnostikos bei perteklinio chirurginio gydymo.
Raktažodžiai: nervų laidumo tyrimai, elektroneuromiografija, riešo kanalo sindromas.
________
* Address: A. Atkočiūnas, M. Marcinkevičiaus ligoninė, Kauno g. 7, Vilnius, Lietuva, LT-03215. Email: aivaras.atkociunas@mmligonine.lt
Received: 14/02/2024. Accepted: 11/03/2024
Copyright © A. Atkočiūnas, A. Šimkutė, R. Mameniškienė, 2023. Published by Vilnius University Press.This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Carpal tunnel syndrome (CTS) is a compressive neuropathy caused by compression of the median nerve in the carpal tunnel, and it is the most common entrapment neuropathy [1,2]. The primary complaints of patients are nocturnal hand paraesthesias, pain and numbness in the distribution of the median nerve, which subsequently extend to diurnal complaints [1,3]. Hand weakness and thenar atrophy occur in the advanced phases of this neuropathy [1]. Well-established risk factors for CTS include age (most commonly, above 50 years old), gender (higher occurrence in women), repetitive monotonous hand movements, anatomical characteristics, such as wrist parameters, medical conditions (rheumatoid arthritis, diabetes, obesity), pregnancy [1,3,4,5].
According to different studies, the prevalence of CTS among adults (aged 15–65) in Western Europe ranged from 0.29% to 43% [6]. Despite well-known risk factors and the wide range of results in studies, numbers show a high prevalence of this disease among people of the working age. Work-related musculoskeletal disorders are the most common group of occupational diseases in Lithuania, accounting for more than 60% of cases [7]. It is estimated that, in European countries, more than 60% of work-related upper extremity musculoskeletal disorders are caused by CTS [3]; meanwhile, mononeuropathies represent more than 10% of occupational disorders in Lithuania [8]. As CTS affects middle-aged active workers, it is associated with high healthcare costs and a hefty economic burden. In a Sweden-based study, researchers found that number of sickness absence and disability pension days were higher among people with CTS than their matched references [9]. Considering the economic burden of the disease, it is of importance to diagnose CTS early and target the patient for further investigation and treatment. In this study, we aimed to evaluate the accuracy of the clinical CTS diagnosis before the nerve conduction studies were performed on the referred patients.
The concordance of clinical diagnoses was assessed by comparing referral diagnoses with the diagnoses confirmed by electroneuromyography. All the patients referred for electroneuromyography between August 2023 and February 2024 were included in the present research. The age and sex, along with the referral and final diagnoses of the patients were taken from their outpatient charts. The obtained data were summarized and processed with Microsoft Office Excel 365, and the data analysis was performed with IBM SPSS Statistics.
Within the initial 6 months since nerve conduction studies and electromyography started to be performed at our hospital, 296 electroneuromyographies were implemented in total. Out of the involved 296 patients, 207 were women (69.9%) and 89 were men (30.1%). The average age of patients was 51.96 ± 15.8 years (19–90 years), and no difference was determined in terms of age between women and men.
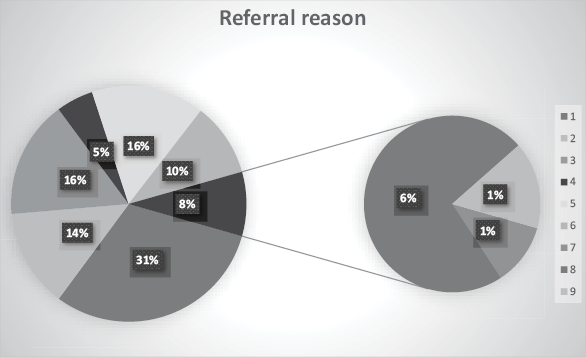
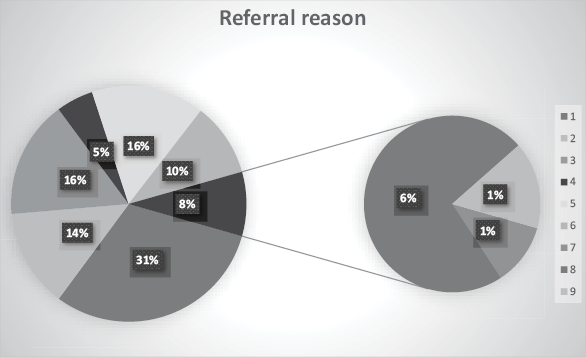
The most common reasons the patients were referred to perform nerve conduction studies (NCS) were the suspected carpal tunnel syndrome (30.7%), cubital tunnel syndrome (13.5%), other upper extremity mononeuropathies (16.2%), and polyneuropathies (15.5%); other groups of referral reasons are presented in Fig. 1.
After performing NCS or NCS with electromyography, the diagnosis was specified for 243 (82.1%) patients, whereas, for 53 (17.9%) patients, no clinically significant changes in the nerve conduction study or myography were determined. The most common diagnosis after consultation was carpal tunnel syndrome (42.6%), followed by pathologies of nerve roots or plexuses (14.5%). Other diagnoses made after electrophysiological evaluation are represented in Fig. 2.
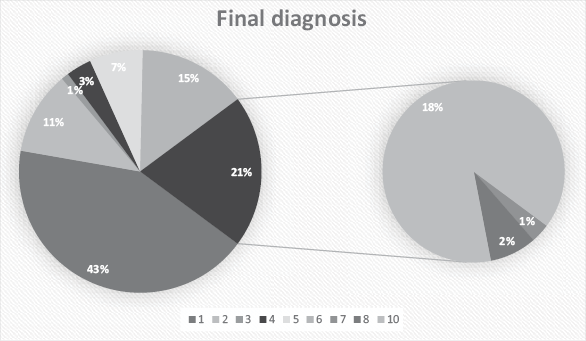
Out of 91 patients referred to electroneurography due to suspicion of CTS, 67 (73.6%) were confirmed cases, whereas, for 12 (13.2%) patients, no abnormalities were detected during NCS. The most common reasons when CTS-positive patients were referred to NCS were CTS in suspicion (53.2%), other upper extremity mononeuropathies (17.5%), cubital tunnel syndrome (10.3%), and polyneuropathies (8.7%).
In the daily clinical practice, the initial diagnosis of CTS is usually made purely on clinical grounds. A combination of symptoms, signs and diagnostic tests should be considered when the diagnosis of CTS is made [10]. The diagnostic value of the history and physical examination findings differ in sensitivity and specificity for Carpal Tunnel Syndrome [11]. In our study, we have found that, after NCS was performed for the referred patients whose CTS diagnosis had been made on the grounds of the medical history and clinical examination alone, only about 74% truly had this condition confirmed. Our findings are similar to the specificity and sensitivity of the classic CTS symptoms reported in the literature.
The classic symptoms of CTS have a specificity of 73% and a sensitivity of up to 75%, which includes pain and paresthesias in the distribution of the median nerve. This involves the palmar aspect of the thumb, index and middle fingers, and the radial half of the ring finger [11]. Nocturnal pain associated with tingling and numbness is only 43-%-specific for this condition [10,11]. Patients often wake up with symptoms and shake out their hands to provide relief. This is known as the flick sign, which is 93%-sensitive and 96%-specific for CTS [11]. Additional clues include positive physical examination findings, such as the Phalen maneuver (reproduction of tingling by having both wrists flexed and held against each other for 1 minute), and the Tinel sign (tapping over the median nerve at the wrist evokes positive sensory symptoms which resemble the patient’s symptoms distal to the wrist) [12]. Although these tests are simple to perform, none of them are diagnostic on their own, but rather complementary to each other, and the combination with NCS is the most reasonable as well as relevant way of diagnosing CTS [10].
Electrodiagnostic studies include nerve conduction studies and electromyography. Sensory NCS is the most sensitive option in electrodiagnostic testing, while motor NCS shows involvement of motor fibers in CTS [13]. Electrodiagnostic studies can also exclude other conditions, such as polyneuropathy and radiculopathy, and assess the severity of CTS [11]. According to different sources of literature, the sensitivity of sensory NCS varies from 73.4% to at least 79.4%, whereas the range of specificity is 93.6–95.7% [13,14]. The sensitivity of distal motor latency for the Median nerve ranges from 56.2% to 71.0%, whereas the specificity of DML was around 95.8%–100% [13,14]. A comparison of the the median to ulnar sensory distal latency by using the 4th finger method can improve the sensitivity and specificity of electrodiagnostic studies to 85.2–92% and 93–100%, respectively [13,15].
One issue with the published literature is that it tends to look at these tests in isolation, rather than combined, which would actually occur in real-life clinical practice [14].
In our hospital, when electroneuromyography is performed for a patient suspected of CTS, in order to achieve the highest possible specificity and sensitivity of the test, not only the traditional CTS criteria are applied (prolonged latency of motor responses, prolonged latencies of sensory responses, and decreased amplitude), but also comparative tests are used, specifically, 4th Finger Median vs Ulnar, and Lumbrical-Interosseous.
Our analysis supports the theory that the electrodiagnostic examination is essential to specify and confirm the diagnosis of CTS, thereby avoiding hyperdiagnostics and preventing patients from excessive surgical treatment.