Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2024, vol. 23(2), pp. 97–107 DOI: https://doi.org/10.15388/LietChirur.2024.23(2).3
Giant Gallstones – a Systematic Review
Amjaad Alkhezzi
Department of Surgery, Unaizah College of Medicine & Medical Sciences, Qassim University, Kingdom of Saudi Arabia
E-mail: amjaadalkhezi@gamil.com
Sajad Ahmad Salati
Department of Surgery, Unaizah College of Medicine & Medical Sciences, Qassim University, Kingdom of Saudi Arabia
E-mail: s.salati@qu.edu.sa
Lamees Sulaiman Alsulaim
Department of Surgery, Unaizah College of Medicine & Medical Sciences, Qassim University, Kingdom of Saudi Arabia
E-mail: dr.lameesz@gmail.com
Mohammad Ahmed Elmuttalut
Department of Community Medicine, Al-Rayan National College of Medicine, Al-Madinah Al-Munawarah, Kingdom of Saudi Arabia
E-mail: motallat@gamil.com
Yasir Ahmed Alsalamah
Department of Surgery, Unaizah College of Medicine & Medical Sciences, Qassim University, Kingdom of Saudi Arabia
E-mail: y.alsalamah@qu.edu.sa
Abstract. Giant gallstones are rare occurrences and measure 5 cm in any one dimension. They present unique set of features and complications. Due to their rarity, we conducted this systematic review to investigate the profile of patients with giant gallstones applying seven variables. For this study, we used the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. After an initial search of 111 peer reviewed articles from reliable sources, we included 29 articles for this study enrolling 30 patients with mean age of 66.7 years. Majority (97%) were symptomatic, reporting with cholecysto-enteric fistula/gallstone ileus (33%), acute cholecystitis (30%) and chronic dyspepsia (24%). The management options adopted included open cholecystectomy (48%), laparoscopic cholecystectomy (33%), endoscopic lithotripsy (6%) and conservative management (6%).
Keywords: giant gallstone, cancer, intestinal obstruction, cholecystectomy, cholecystoenteric fistula, Bouveret syndrome.
Received: 2024-02-29. Accepted: 2024-04-12.
Copyright © 2024 Amjaad Alkhezzi, Sajad Ahmad Salati, Lamees Sulaiman Alsulaim, Mohammad Ahmed Elmuttalut, Yasir Ahmed Alsalamah. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Gallstones constitute a significant health problem particularly in the developed societies, affecting about 10% to 20% of the adult population [1]. Majority of gallstones (80%) are clinically “silent”, and discovered incidentally during an abdominal ultrasound conducted for some other reason [2]. Expectant management is currently considered as an appropriate choice for such silent gallstones as only 2% to 3% per year develop symptoms (biliary pain) that require treatment and an even lower proportion, 1% to 2% per year, develop major gallstone complications like cholecystitis, pancreatitis, choledocholithiasis, ascending cholangitis, cholecystoenteric fistulae, or perforation. However, the bigger sized gallstones tend to display a different behaviour. They have been positively corelated with gallbladder cancer [3–5] and can potentially lead to pressure necrosis of gallbladder wall, thereby resulting into fistulization into the adjacent viscera [6, 7]. Furthermore, during cholecystectomy they pose technical challenges, as it is difficult to grasp the gallbladder with laparoscopic instruments and expose the anatomy of Calot’s triangle.
“Large stones” are commonly defined as stones larger than 3 cm in any one dimension, and “giant stones”, a rarer variant, have been generally defined as stones larger than 5 cm though, there is no clear consensus in literature over the measurements to be used to define a gallstone as “giant” or “large” [8–10].
It is against this backdrop that this systematic meta-analysis of recently published reports in peer reviewed literature was carried out to elucidate the important characteristics associated with giant gallstones.
Materials and methods
Methods. Systematic literature search was conducted through electronic databases, including PubMed, Science Direct, ResearchGate, Google Scholar and Scopus using the key-words “giant gallstones”, “large gallstones”, “big gallstones” by four authors. The search was carried out by using individual keywords with a combination of Boolean Logics (AND). Furthermore, only reports that were published in English were considered for inclusion in this study. Timeframe fixed for inclusion of studies was 2010–2022.
Criteria for considering studies. Articles including case series and case reports were included for the review process. No original article was found in literature that could satisfy the criteria of inclusion.
Participants and Outcome measures. Only those cases were included where the dimension of at least one side of gallstone was documented to be 5 cm. The following seven variables (Table 1) were reported and analysed: (I) age of the patient, (II) gender, (III) clinical presentation, (IV) management, (V) size of the gallstones, (VI) number of gallstones, (VII) presence/absence of malignancy.
Exclusion. All such articles or individual cases in the case series were excluded where the size of gallstone was less than 5 cm, even though such smaller sized stones were labelled as giant gallstones. Articles in language other than English were also excluded.
Methodological quality checking. Checklist items used in well cited studies were selected randomly and compared with the checklist self-drafted for this systematic review.
Data extraction and analysis. Data on the number of cases and the seven variables were retrieved (Table 1). Microsoft Excel (Office Version 16) and the Statistical Package for Social Sciences (IBM-SPSS version 27.0) were used to enter and analyse the obtained data. Simple frequencies, measures of central tendency, and measures of variability were utilized in descriptive statistical studies to describe participant characteristics.
The data was then presented as indicated by the results using frequencies, summary measures, tables, and figures. P < 0.05 and a 95% confidence interval were used to determine the statistical significance of the difference. High-quality research that reported on the efficacy and made recommendations for clinical application were used to draw the conclusion.
Results
Study selection. The electronic database search resulted in a total of 111 articles from five sources as shown in Table 1. After excluding 74 duplicated articles, 37 case reports were used to screen titles and abstracts, after which, 37 potentially relevant articles in English language were assessed for the eligibility criteria. Finally, 29 articles were included in the review after fulfilment of inclusion criteria as shown in Table 1.
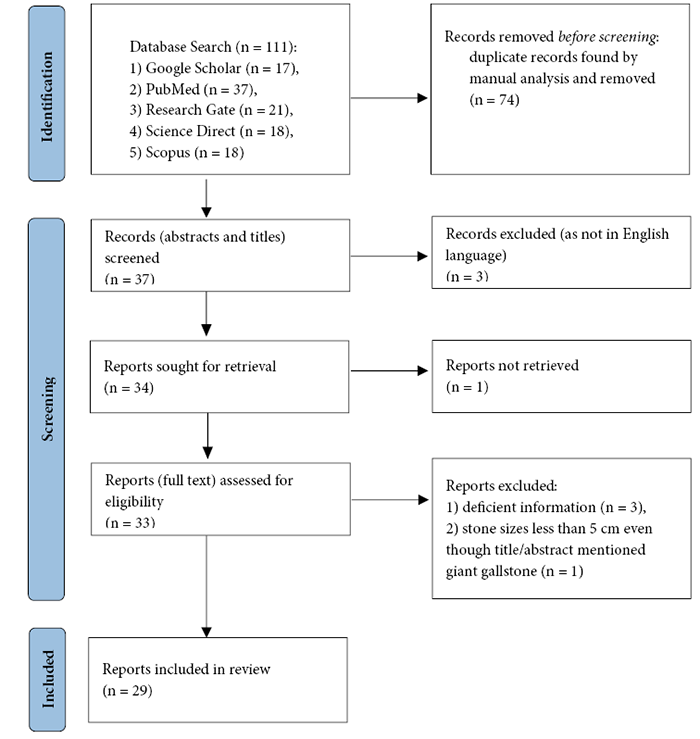
Figure 1. Flowchart of the reviewed articles
Study characteristics. Study characteristics are summarized in Table 1. There were 29 articles including 28 single case reports, and 1 case series (with two cases) satisfying the inclusion criteria. The two-case series [11, 12] had only one case each that satisfied the inclusion criteria and hence were considered as single case reports.
There was a total of 30 cases including 21 (70%) females and 9 (30%) males ranging in age from 11 to 90 (mean 66.7) years. Only 1 (3%) asymptomatic patient had been detected incidentally while being imaged for unrelated problems. 10 (30%) patients had reported as acute cholecystitis, 11 (33%) patients had cholecysto-enteric fistula/gallstone ileus and 8 (24%) cases presented with chronic dyspepsia/biliary colics. The management options adopted included laparoscopic cholecystectomy (LC) in 10 (33%) cases which is currently the gold standard of management for cholelithiasis. In 16 patients, open surgery had been adopted; in 9 (27%) cases, open cholecystectomy had been pre-planned whereas in 7 (21%), LC had been started but converted to open due to difficulties. Endoscopic lithotripsy had been successfully conducted in 2 (6%) cases and conservative management had been adopted in 2 (6%) cases.
Giant stones were solitary in 28 (94%) and in 2 (6%) cases, there were multiple stones, out of which at least one was giant. The greatest dimension of gallstones ranged between 5 cm and 16.8 cm (mean 7.89 cm). Malignancy was neither reported on the basis of preoperative workup nor after histopathological analysis of retrieved gallbladder specimens in any of the cases (0%).
Table 1. Patient characteristics in included articles
|
Serial number |
Series |
Year of publication |
Number of patients |
Gender (M/F) |
Age (years) |
Clinical |
Management |
Size of gallstone (in centimetres) |
Solitary stone |
Malignancy (preoperative diagnosis/histopathology report) |
Additional Remarks |
|||||||
|
Asymptomatic |
Acute cholecystitis |
Chronic dyspepsia/Biliary colics |
Cholecysto-enteric fistula/gallstone ileus |
Laparoscopic Cholecystectomy (LC) |
Open Surgery |
LC converted to open |
Endoscopic Lithotripsy |
Conservative |
||||||||||
|
1. |
Demircioğlu et al. [9] |
2022 |
1 |
F |
83 |
|
|
7 x 5 x 4 |
|
Cholecystoduodenal fistula; gut obstruction with hemodynamic instability leading to cardiac arrest and revival by cardiopulmonary resuscitation followed by laparotomy and enterotomy to extract the giant gallstone. |
||||||||
|
2. |
Khan et al. [10] |
2022 |
1 |
F |
69 |
|
|
9 |
|
The manipulation of gallbladder was carried out using opened jaws of a bowel grasper, the so called “Fan technique”. |
||||||||
|
3. |
Alhebshi et al. [13] |
2022 |
1 |
F |
42 |
|
|
7 x 4 |
|
Obscured Calot’s triangle anatomy due to giant stone resulted in conversion to open cholecystectomy. |
||||||||
|
4. |
Rashid et al. [14] |
2021 |
1 |
M |
63 |
|
|
7 x 2.5 |
|
Obscured Calot’s triangle anatomy due to giant stone resulted in conversion to open cholecystectomy. |
||||||||
|
5. |
Shrestha et al. [11] |
2021 |
1 |
F |
39 |
|
|
5 x 3 x 2.8 |
|
Two cases reported in this series, only one included in this review due to the size above 5 cm. |
||||||||
|
6. |
Al-Mulla et al. [15] |
2021 |
1 |
M |
38 |
|
|
7 x 4 |
|
--- |
||||||||
|
7. |
Mahoney et al. [16] |
2021 |
1 |
M |
53 |
|
|
12.2 x 5.2 x 5.2 |
|
The critical view of safety could not be achieved in LC due to the severe inflammation as well as limited gallbladder mobility because of the enormous stone; hence converted to open. |
||||||||
|
8. |
Goonawardhana et al. [17] |
2021 |
1 |
F |
90 |
|
|
6 × 3 |
|
Bouveret syndrome managed with endoscopic lithotripsy but gallstone fragments led to small bowel obstruction requiring laparotomy. |
||||||||
|
9. |
Igwe & Diri [8] |
2020 |
2 |
F |
32 |
|
|
8.2 x 7.5 |
|
--- |
||||||||
|
F |
62 |
|
|
8 x 6 |
× |
Multiple calculi with one measuring 8 cm by 6 cm. |
||||||||||||
|
10. |
Nguyen et al. [18] |
2020 |
1 |
F |
85 |
|
|
9 × 6 |
|
Duodenal obstruction (Bouveret syndrome); treated with a radical one-stage procedure: fistulotomy for gallstone removal, cholecystectomy, side-to-side Roux-en-Y duodenojejunostomy. |
||||||||
|
11. |
Chan et al. [19] |
2020 |
1 |
M |
71 |
|
|
7.5 |
|
Incidental finding in CT scan done for other purpose. |
||||||||
|
12. |
Parvataneni et al. [7] |
2020 |
1 |
F |
85 |
|
|
5 x 4.5 |
|
Bouveret syndrome masquerading as a gastric mass; managed with endoscopic luminal laser lithotripsy. |
||||||||
|
13. |
Al Zoubi et al. [12] |
2020 |
1 |
F |
44 |
|
|
6 × 4 × 3.3 |
|
Three cases reported in this series, only one included in this review due to the size above 5 cm. |
||||||||
|
14. |
Sampath et al. [20] |
2020 |
1 |
F |
40 |
|
|
7.5 x 3 |
|
Patient had reported with acute pancreatitis; ERCP and wide sphincterotomy with CBD stenting followed by LC done. |
||||||||
|
15. |
Singh et al. [21] |
2020 |
1 |
F |
72 |
|
|
12.8 x 7 |
|
Largest gallstone to be removed laparoscopically in the world. |
||||||||
|
16. |
Sharma et al. [22] |
2019 |
1 |
F |
64 |
|
|
8 x 4.4 x 4.1 |
|
--- |
||||||||
|
17. |
Hajjar et al. [6] |
2018 |
1 |
M |
73 |
|
|
5 × 7 |
|
Cholecystocolonic fistula, presented with haematochezia and intestinal obstructive symptoms; laparotomy and colotomy done. |
||||||||
|
18. |
Macías et al. [23] |
2018 |
1 |
M |
63 |
|
|
10 x 5 |
|
Bouveret syndrome with obstruction in second part of duodenum. |
||||||||
|
19. |
Gallego Otaegui et al. [24] |
2016 |
1 |
F |
84 |
|
|
8 x 4 x 3 |
|
Bouveret syndrome. |
||||||||
|
20. |
De Giorgi et al. [25] |
2015 |
1 |
F |
83 |
|
|
5 × 2 |
× |
|
Gallstone ileus but surgery not done due to medical contraindications; treated conservatively and gallstones evacuated with stools spontaneously. |
|||||||
|
21. |
Kaul & Kaul [26] |
2015 |
1 |
F |
11 |
|
|
8 x 3 |
× |
Adhesions and distorted anatomy led to conversion of LC into Open; multiple gallstones, with one being giant. |
||||||||
|
22. |
Dalal et al. [27] |
2014 |
1 |
F |
38 |
|
|
7.4 x 5.4 |
|
Elective open cholecystectomy for giant gallstone. |
||||||||
|
23. |
Qasaimeh et al. [28] |
2014 |
1 |
M |
70 |
|
|
5.0 × 3.5 |
|
Bouveret’s syndrome; endoscopic management failed; open surgical treatment successful. |
||||||||
|
24. |
Banigo [29] |
2013 |
1 |
F |
57 |
|
|
6 × 3.5 × 3 |
|
Technical difficulties led to conversion of LC into Open. |
||||||||
|
25. |
Salemans et al. [30] |
2013 |
1 |
F |
78 |
|
|
6 |
|
Failed conservative management for sigmoid colonic obstruction followed by laparotomy and re-laparotomy; patient died. Multiple co-morbidities due to which conservative option had been adopted. |
||||||||
|
26. |
Xu et al. [31] |
2013 |
1 |
M |
70 |
|
|
9.5 x 6 x 4.5 |
|
Subxiphoid trocar incision was extended to extract the gallbladder (with giant stone) in specimen retrieval bag. |
||||||||
|
27. |
Becerra et al. [32] |
2011 |
1 |
M |
57 |
|
|
16.8 x 7.8 x 4.1 |
|
Largest gallstone by volume (in literature); fresh weight (at operation) was 278.0 g and, after 4 years, its dry weight was 259.5 g. |
||||||||
|
28. |
Bajradharya et al. [33] |
2011 |
1 |
F |
67 |
|
|
6 x 4 |
|
Colonic gallstone ileus, managed conservatively and gallstone evacuated with stools spontaneously. |
||||||||
|
29. |
Zea et al. [34] |
2010 |
1 |
F |
45 |
|
|
10 × 4 × 4 |
|
Caused a palpable lump in right hypochondrium that was initially misdiagnosed as cancer; the weight of the giant gallstone was 110 grams. |
||||||||
Discussion
Gallstones are a major health concern, especially in affluent societies but majority of them (80%) are clinically “silent”, and are treated expectantly [1–2]. In literature, there is no clear consensus over the precise dimension beyond which a gallstone may be labelled as large or giant but generally gallstones greater than 3 cm in any one dimension are termed as “large stones” whereas the stones larger than 5 cm are termed as “giant gallstones” [8–10]. In this review, as 5 cm was adopted by the authors as the threshold dimension for inclusion as giant stone, only one case was included from the series by Zoubi et al. [12] and two cases with gallstones lesser than 5 cm (4.5 cm and 4.1 cm) were excluded. Different sized giant gallstones have been reported in the literature and most of them are solitary. Singh et al. [21] reported a gallstone measuring 12.8 cm x 7 cm and this is mentioned in literature, as the largest gallstone removed through laparoscopic. Otherwise, a giant gallstone measuring 16.8 cm x 7.8 cm x 4.1 cm and weighing 278.0 g was removed by classical open cholecystectomy by Becerra et al. [32]. Igwe and Diri [8] in their report of two cases that were successfully managed by laparoscopic cholecystectomy, recovered a solitary giant gallstone measuring 8.2 cm x 7.5 cm in first case whereas in the second case, there were multiple calculi, one of them being giant with dimensions of 8 cm x 6 cm.
Out of the 30 cases included in this review, 29 (97%) has reported with symptoms and only 1 (3%) case was asymptomatic at incidental detection. 10 (33%) patients had cholecystoenteric fistula/gallstone ileus. As the size of gallstones increase, the pressure exerted in the gallbladder wall increases, leading gradually to pressure necrosis and thereby resulting in cholecystoenteric fistula through which the gallstone passes and causes intestinal obstruction [6–7]. Out of the 11 cases of cholecystoenteric fistula/gallstone ileus, 6 (18%) had cholecystoenteric fistula/gallstone ileus presented with Bouveret syndrome. Bouveret’s syndrome refers to gastric outlet obstruction caused by large gallstones that get lodged in the duodenal bulb after migrating through a fistula between gallbladder and stomach or duodenum and in literature, typically has been described in elderly patients with multiple medical comorbidities. In this review, the age of the patients presenting with Bouveret syndrome ranged 63–90 years (mean 79.5 years; mode 85 years) and thereby concur with the literature.
Laparoscopic cholecystectomy (LC) is currently considered the criterion standard for the treatment of symptomatic cholelithiasis and this approach results in lesser postoperative pain, better cosmetic outcomes, and shorter hospital stays and disability from work than open cholecystectomy [35]. However, in case of giant gallstones, due to multiple difficulties appearing during LC, open approach still holds an important role. Firstly, the bigger stones usually lead to inflammation that thickens the gallbladder wall and Raman et al. [36] by their bivariate analysis have demonstrated a significant correlation between conversion of LC to open surgery and the gallbladder wall thickness. Secondly, due to presence of giant stone, it is highly challenging to grasp the gallbladder with the available laparoscopic tools and dissect safely to obtain the proper anatomical exposure of Calot’s triangle, particularly when operation is performed in the setting of acute cholecystitis [10]. Furthermore, the giant stone due to pressure leads to a stretched-out wall and later the fistula formation, making dissection tricky. And at the end of the procedure, the retrieval of the gallbladder specimen along with the giant stone poses technical difficulties due to size mismatch with the 10–11 mm port sites and often requires suitable extension of the incision. However, even with the giant gallstones, in the hands of the skilled laparoscopic surgeons, LC is the being published as best initial course of action. In this review, the authors found that laparoscopic cholecystectomy (LC) had been adopted in 10 (33%) whereas in 9 (27%) cases, open cholecystectomy had been pre-planned and in 7 (21%), LC had been converted to open.
When it comes to non-operative expectant management, De Giorgi et al. [25] and Zea et al. [34] had managed their respective cases by this option, but the decision had been taken due to medical contraindications, and gallstone ileus got resolved as gallstones evacuated with stools spontaneously. Salemans et al. [30] had on similar grounds adopted conservative management for sigmoid colonic obstruction caused by giant gallstone, and that option had failed and laparotomy and re-laparotomy was conducted but the patient had died. As otherwise, in contrast to the smaller sized gallstones where expectant management is offered, early elective cholecystectomy should be recommended for appropriate patients, when giant gallstones are identified, due to the high potential for complications [16].
Endoscopic lithotripsy had been successfully conducted in 2 (6%) cases of Bouveret syndrome and this is a recent innovation in this field. In a case reported by Goonawardhana et al. [17], a 90-year-old female with Bouveret syndrome and CT-proven 6 cm giant stone in third part of duodenum, declined surgical intervention and was hence subjected to endoscopic lithotripsy but a 4 cm gallstone fragment led to distal small bowel obstruction requiring laparotomy. Parvataneni et al. [7] reported an 85-year-old female patient with Bouveret syndrome due to a 5 cm impacted gallstone in the duodenal bulb, masquerading as a gastric mass; endoscopic nets and baskets were unsuccessful in removal of the stone, and given her advanced age, poor physical condition and underlying comorbidities, she was deemed unfit for surgical intervention. Hence, endoscopic laser lithotripsy was successfully attempted. There were no post-procedure complications and the patient experienced complete resolution of her symptoms.
In literature, the increased size of gallstones is positively corelated with the development of adenocarcinoma of gallbladder [3–5, 37–40]. Lowenfels et al. [37] after analysis of histopathology reports of cholecystectomy specimen from 1 676 subjects from various races found that the relative risk for gallbladder cancer in subjects with gallstones greater than or equal to 3 cm was 9.2 compared with subjects with stones less than 1 cm (95% confidence interval: 2.3–37). They estimated that one-third of all gallbladder cancers in subjects with gallstones would be associated with large (greater than or equal to 3 cm) stones and stressed that the size of gallstones can be used to determine the risk of gallbladder cancer. But none of the cases in our study, had imaging or histopathology reports suggestive of cancer.
Conclusion
Giant gallstones exceeding 5 cm are rare occurrences and carry a higher risk of complications including biliary enteric fistula, ileus, and gallbladder cancer and hence, cholecystectomy should be recommended, even if they are asymptomatic. Laparoscopic cholecystectomy in the hands of a skilled surgeon, appears to be the treatment of choice though the giant stone poses technical challenges. Conversion of LC to open cholecystectomy in case of failure to obtain the “critical view of safety” or else a planned open surgery is not to be considered a failure. Endoscopic lithotripsy appears promising, particularly when there is a high-risk for surgical intervention. There is a need for clear consensus upon the definition of giant gallstones as there is still no uniform way of using the phrase in literature.
Funding. The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests. None declared.
References
1. Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver 2012; 6(2): 172–187. DOI: 10.5009/gnl.2012.6.2.172.
2. Halldestam I, Enell EL, Kullman E, Borch K. Development of symptoms and complications in individuals with asymptomatic gallstones. Br J Surg 2004; 91(6): 734–738. DOI: 10.1002/bjs.4547.
3. Roa I, Ibacache G, Roa J, Araya J, de Aretxabala X, Muñoz S. Gallstones and gallbladder cancer-volume and weight of gallstones are associated with gallbladder cancer: a case-control study. J Surg Oncol 2006; 93(8): 624–628. DOI: 10.1002/jso.20528.
4. Shrikhande SV, Barreto SG, Singh S, Udwadia TE, Agarwal AK. Cholelithiasis in gallbladder cancer: coincidence, cofactor, or cause! Eur J Surg Oncol 2010; 36(6): 514–519. DOI: 10.1016/j.ejso.2010.05.002.
5. Huang D, Joo H, Song N, Cho S, Kim W, Shin A. Association between gallstones and the risk of biliary tract cancer: a systematic review and meta-analysis. Epidemiol Health 2021; 43: e2021011. DOI: 10.4178/epih.e2021011.
6. Hajjar R, Létourneau A, Henri M, Heyen F, Latulippe JF, Poirier M, Tremblay JF, Trépanier JS, Bendavid Y. Cholecystocolonic fistula with a giant colonic gallstone: the mainstay of treatment in an acute setting. Journal of Surgical Case Reports 2018; 10: 1–3. DOI: 10.1093/jscr/rjy278.
7. Parvataneni S, Khara HS, Diehl DL. Bouveret syndrome masquerading as a gastric mass-unmasked with endoscopic luminal laser lithotripsy: a case report. World J Clin Cases 2020; 8(22): 5701–5706. DOI: 10.12998/wjcc.v8.i22.5701.
8. Igwe PO, Diri ON. Laparoscopic cholecystectomy for giant gall stone: report of two cases. Int J Surg Case Rep 2020; 67: 207–210. DOI: 10.1016/j.ijscr.2020.01.055.
9. Demircioğlu M, Demircioğlu Z, Önal C, Özler S. Difficult management of giant gallstone ileus of a post-cardiopulmonary resuscitation patient: a case report. Cureus 2022; 14(4): e23911. DOI: 10.7759/cureus.23911.
10. Khan IJ, Alahmad M, Aurif F, Mir NH. Laparoscopic cholecystectomy for a giant gallstone. Arch Clin Med Case Rep 2022; 6(1): 40–44. DOI: 10.26502/acmcr.96550447.
11. Shrestha A, Bhattarai S, Shrestha S, Chand M, Bhattarai A. Laparoscopic cholecystectomy for large/giant gallstones: case report and brief review of literature. Nepal Mediciti Medical Journal 2021; 2(2): 87–90. DOI: 10.3126/nmmj.v2i2.41283.
12. Al Zoubi M, El Ansari W, Al Moudaris AA, Abdelaal A. Largest case series of giant gallstones ever reported, and review of the literature. Int J Surg Case Rep 2020; 72: 454–459. DOI: 10.1016/j.ijscr.2020.06.001.
13. Alhebshi AH, Haddad FM, Alsharif GG, Zeid GA. Giant gallstone, rare cause for conversion to open cholecystectomy from laparoscopic. Ann Clin Med Case Rep 2022; 8(16): 1–3. https://acmcasereport.com/wp-content/uploads/2022/04/ACMCR-v8-1757.pdf
14. Rashid T, Altaf J, Husain M. A case of a large/giant gallbladder stone retrieved during cholecystectomy at a tertiary care centre in North India with review of literature. IAR J Med Cse Rep 2021; 2(3): 32–34. DOI: 10.47310/iarjmcr.2021.v02i03.007.
15. Al-Mulla AE. Laparoscopic removal of giant gallbladder stone: a rare case report in Kuwait. RAS Medical Science 2021; 1(3): 1–2. http://www.raspublishers.com/articles?id=50
16. Mahoney RC, Marison SR Jr, Marumoto AD, Hemmings DE. Enormous gallstone discovered in the setting of acute-on-chronic cholecystitis. Hawaii J Health Soc Welf 2021; 80(11 Suppl 3): 38–40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8609192/
17. Goonawardhana D, Huynh R, Rabindran J, Becerril-Martinez G. Endoscopic lithotripsy for Bouveret syndrome complicated by small bowel obstruction secondary to gallstone fragments. Journal of Surgical Case Reports 2021; 4: 1–3. DOI: 10.1093/jscr/rjab118.
18. Nguyen BH, Le Quan AT, Hai PM, Quang Hung V, Thai TT. Duodenal obstruction due to giant gallstone: a case report. Int Med Case Rep J 2020; 13: 651–656. DOI: 10.2147/IMCRJ.S278058.
19. Chan AW, Sabaratnam RM, Pillay Y. Massive gallstone in an asymptomatic Indigenous Canadian male: case report and literature review. Int J Surg Case Rep 2020; 72: 429–432. DOI: 10.1016/j.ijscr.2020.06.028.
20. Sampath K, Kannan R, Indira G, Arun M. Giant gallbladder calculi with biliary pancreatitis – a rare case report. International Journal of Scientific Research 2020; 9(8): 53–54. DOI: 10.36106/ijsr.
21. Singh Y, Mohammed S, Hosein A, Ramoutar K, Naraynsingh V. A giant gallstone: the largest gallstone removed laparoscopically in the world. Cureus 2020; 12(5): e7933. DOI: 10.7759/cureus.7933.
22. Sharma V, Kaundal V, Sharma A, Singh G, Shah P, Kapoor A. Giant gall stone: a rare finding performed with open cholecystectomy. Int Surg J 2019; 6(2): 630–632. DOI: 10.18203/2349-2902.isj20190420.
23. Macías L, Rocha A, Alvarado M, Chung J, Yépez D. Bouveret syndrome, a rare form of gallstone ileus. Case Reports 2018; 4(1): 39–45. DOI: 10.15446/cr.v4n1.65771.
24. Gallego Otaegui L, Sainz Lete A, Gutiérrez Ríos RD, Alkorta Zuloaga M, Arteaga Martín X, Jiménez Agüero R, Medrano Gómez MÁ, Ruiz Montesinos I, Beguiristain Gómez A. A rare presentation of gallstones: Bouveret’s syndrome, a case report. Rev Esp Enferm Dig 2016; 108(7): 434–436. https://scielo.isciii.es/pdf/diges/v108n7/imagenes3.pdf
25. De Giorgi A, Caranti A, Moro F, Parisi C, Molino C, Fabbian F, Manfredini R. Spontaneous resolution of gallstone ileus with giant stone: a case report and literature review. J Am Geriatr Soc 2015; 63(9): 1964–1965. DOI: 10.1111/jgs.13635.
26. Kaul N, Kaul V. A rare case of giant gall stone in a young prepubertal female. Journal of Evolution of Medical and Dental Sciences 2015; 4(44): 7695–7698. DOI: 10.14260/jemds/2015/1119.
27. Dalal S, Pankaj, Bhoriwal S, Kumar R, Sujata. Giant gallstone: a rare indication of open cholecystectomy. Journal of Case Reports 2014; 4(1): 17–19. DOI: 10.17659/01.2014.0005.
28. Qasaimeh GR, Bakkar S, Jadallah K. Bouveret’s syndrome: an overlooked diagnosis. A case report and review of literature. Int Surg 2014; 99(6): 819–823. DOI: 10.9738/INTSURG-D-14-00087.1.
29. Banigo A. Huge gallstone complicating laparoscopic cholecystectomy. Case Reports 2013; 2013. DOI: bcr2012007012.
30. Salemans PB, Vles GF, Fransen S, Vliegen R, Sosef MN. Gallstone ileus of the colon: leave no stone unturned. Case Reports in Surgery 2013; 359871: 5. DOI: 10.1155/2013/359871.
31. Xu X, Hong T, Zheng C. Giant gallstone performed by emergency laparoscopic cholecystectomy. Int J Surg Case Rep 2013; 4(12): 1163–1164. DOI: 10.1016/j.ijscr.2013.10.002.
32. Becerra P, Becerra V, Aguilar C, Modragon I, Cooper DK. Giant gallstone: a case report. Int J Surg Case Rep 2011; 2(7): 228–229. DOI: 10.1016/j.ijscr.2011.07.005.
33. Bajradharya A, Pathania OP, Adhikary S, Agrawal CS. A case of colonic gallstone ileus with a spontaneous evacuation. Health Renaissance 2011; 9(1): 47–49. DOI: 10.3126/hren.v9i1.4363.
34. Zea MI, Anees A, Khan M. A giant gall stone presenting as hard lump: a case report. Middle East Journal of Internal Medicine 2010; 3: 48–50. http://www.me-jim.com/NewArchives/MEJIM_Vol3_Iss1.pdf
35. Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, Leandro G, Montori G, Ceresoli M, Corbella D, Sartelli M, Sugrue M, Ansaloni L. Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg 2015; 18: 196–204. DOI: 10.1016/j.ijsu.2015.04.083.
36. Raman SR, Moradi D, Samaan BM, Chaudhry US, Nagpal K, Cosgrove JM, Farkas DT. The degree of gallbladder wall thickness and its impact on outcomes after laparoscopic cholecystectomy. Surg Endosc 2012; 26(11): 3174–3179. DOI: 10.1007/s00464-012-2310-8.
37. Lowenfels AB, Walker AM, Althaus DP, Townsend G, Domellöf L. Gallstone growth, size, and risk of gallbladder cancer: an interracial study. Int J Epidemiol 1989; 18(1): 50–54. DOI: 10.1093/ije/18.1.50.
38. Pang Y, Lv J, Kartsonaki C, Guo Y, Yu C, Chen Y, Yang L, Bian Z, Millwood IY, Walters RG, Li X, Zou J, Holmes MV, Chen J, Chen Z, Li L. Causal effects of gallstone disease on risk of gastrointestinal cancer in Chinese. Br J Cancer 2021; 124(11): 1864–1872. DOI: 10.1038/s41416-021-01325-w.
39. Hsing AW, Gao YT, Han TQ, Rashid A, Sakoda LC, Wang BS, Shen MC, Zhang BH, Niwa S, Chen J, Fraumeni JF Jr. Gallstones and the risk of biliary tract cancer: a population-based study in China. Br J Cancer 2007; 97(11): 1577–1582. DOI: 10.1038/sj.bjc.6604047.
40. Zou S, Zhang L. Relative risk factors analysis of 3,922 cases of gallbladder cancer. Zhonghua Wai Ke Za Zhi 2000; 38(11): 805–808.